Study Procedure
All consecutive patients indicated for elective reverse total shoulder arthroplasty will be considered eligible. After reading the information sheet and signing the consent form, they will be enrolled. Baseline characteristics of age, sex, hand dominance, medications, body mass index, prior surgeries, alcohol/tobacco use, and relevant comorbidities will be recorded in a deidentified Patient Data Form (PDF) along with arthritis type, associated arthritis characteristics based on pre-operative X-rays and CT scan, pre-operative range of motion, Constant Score, and scores from 2 x Patient Reported Outcome Measures (PROMs): the American Shoulder and Elbow Society Score – Patient and the Pain and Normal Visual Analog Score.
Stage 1
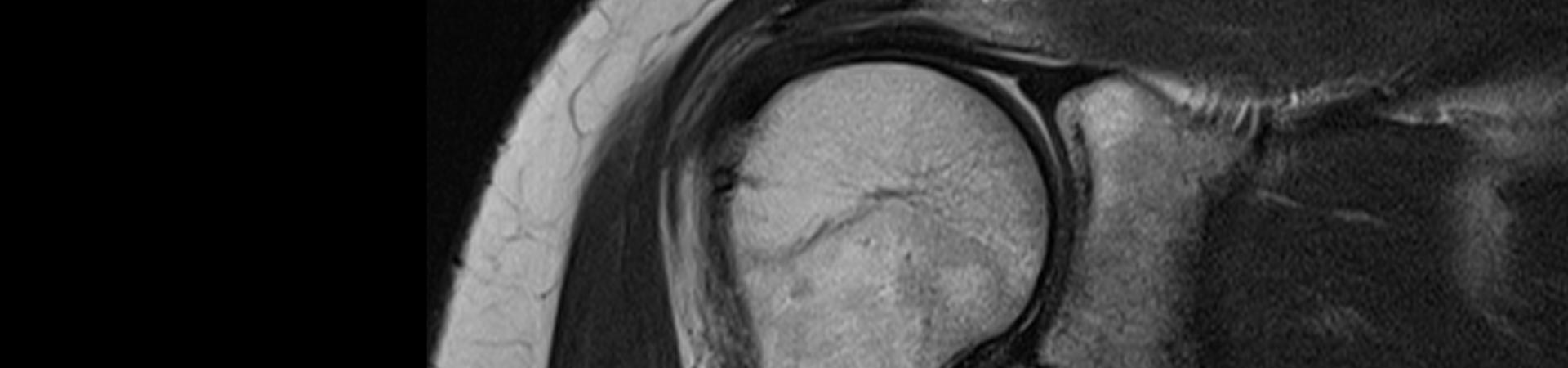
In stage 1 of the study, the first 40 patients enrolled in the study will undergo reverse total shoulder arthroplasty with two-dimensional (2D) preoperative planning (radiographs and CT scan) and using standard manufacturer instrumentation (sRSA) with the Zimmer Biomet Comprehensive Reverse Total Shoulder Arthroplasty system (Biomet Orthopaedics, Warsaw, Indiana, USA). This is how the principal investigator performs his surgeries currently. The next 40 patients enrolled in the study will undergo reverse total shoulder arthroplasty with three-dimensional (3D) preoperative planning (X-rays, CT scans, and 3D reconstruction) and using patient specific instrumentation (pRSA) with the Zimmer PSI Shoulder system and Signature ONE planning software. The next 40 patients enrolled in the study will undergo reverse total shoulder arthroplasty with 3D preoperative planning (X-rays, CT scans, and 3D reconstruction) and using intraoperative computer navigation (cRSA) with the Zimmer Biomet Comprehensive Reverse Total Shoulder Arthroplasty system and Signature ONE planning software.
The surgery will proceed with the surgeon performing sRSA, pRSA, or cRSA for the patient’s shoulder arthritis depending on the patient’s predetermined enrolment. The rotator cuff status, implant size, use of augmentation or bone graft, and operative time will be documented. After the surgery, the patient will be admitted to the hospital for routine postoperative care. A postoperative CT scan of the shoulder will be obtained to measure implant position and accuracy of the preoperative planning and instrumentation used for implantation. The patient will be discharged from the hospital depending on pain control and medical status. They will follow-up in clinic at 2 weeks, 4 months, 1 year, and 2 years from surgery.
The primary outcome will be range of motion. Secondary outcomes will be scores on the Constant Score, the American Shoulder and Elbow Society Score – Patient, the Pain and Normal Visual Analog Score and the Patient Satisfaction Post Op Score as well as implant position, and any complications.
All outcomes will be documented on the PDF. Postoperative shoulder X-rays will be obtained at each clinic visit to evaluate for implant position, fracture, dislocation, scapular notching, or implant loosening. All data will be collated and analysed.
As not all technologies are immediately available in 2021, the decision was made to do a non-randomised study first (Stage 1). The cRSA will be available in Australia in early 2022. Therefore, stage 1 will allow patients to be enrolled in the sRSA and pRSA groups. Then a randomised study (Stage 2) will be performed once all techniques are available and the surgeon and staff are equally experienced in their use. Also, the randomised trial can correct for any timeline bias in the first study (Stage 1). If there is no significant bias (change in patient characteristics, non-randomisation process, or increasing surgical experience with the technique) in Stage 1, some outcomes may be combined from Stage 1 and Stage 2 for additional statistical analyses.
Stage 2
In stage 2 of the study, all consecutive patients indicated for elective reverse total shoulder arthroplasty will be considered eligible. After reading the information sheet and signing the consent form, they will be randomised to one of 3 study groups: sRSA, pRSA, or cRSA. Patients will be randomly assigned to groups by the use of sealed and numbered envelopes opened at the time their surgery is booked. Inside their envelopes are instructions for which group patients will be assigned.
Randomisation will be done using computer software to generate the numbers for the envelopes. This will be a single-blinded study. The patient will be blinded to the type of technology used for their RSA. The surgeon will not be blinded to which groups patients are assigned because he needs this information in order to perform the surgery with the indicated instrumentation. The pre-operative data collection, surgery, and post-operative data collection will be performed in the same was as in Stage 1.