Objectives
The primary objective of the Study was to demonstrate that the clinical outcome of the healing rate of the tendons is the same between the 2 rehabilitation protocols i.e. the traditional protocol with 6 weeks immobilization and our early mobilization protocol with 2 weeks immobilization.
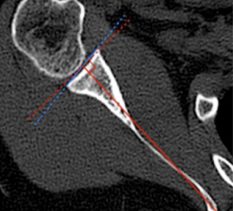
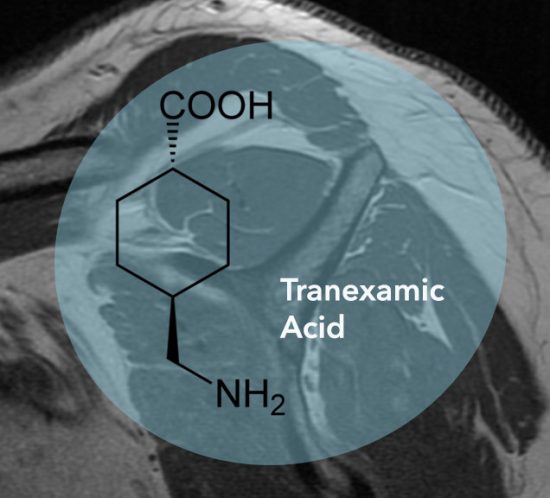
Integrity of repair on MRI at 6 months was the primary means of measuring outcome. Secondary measurement was via standardized assessments of the shoulder and general quality-of-life assessments at baseline and 6 months.
Design
This was a pilot prospective cohort study that enrolled 20 patients over a one year period.
Study Procedure
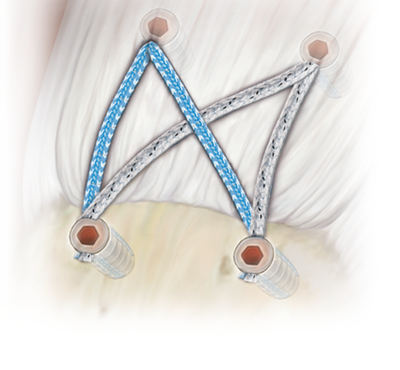
Patients had their shoulders immobilized in a standard abduction immobilization sling for 2 weeks. No mobilization and no physiotherapy of the shoulder was authorized during this time. Self-directed mobilization of the elbow, wrist, and hand was performed. The sling was removed at the beginning of the third week post-surgery and gentle activities of daily living (e.g. reading, eating, showering, typing etc.) permitted. The patients were specifically advised against lifting more than 1kg, attempted use of the arm at shoulder height or above, pushing, reaching or climbing. At week 6 post-surgery, a passive and active assisted range of motion protocol was introduced and supervised by a physiotherapist. A strengthening program was introduced at 3 months following surgery. Return to full unrestricted activities was anticipated at 6 months. Standard, functional parameters, patient outcome measures (Constant-Murley Shoulder Score, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) and Veterans Rand 36 General Health Survey) and MRI scans were assessed pre-operatively, and post-operatively at 6 months. MRI scans were analysed by a single radiologist for the whole Study group.
Ethics and Governance
Approved by North Shore Private Hospital Human Research Ethics Committee to be undertaken at North Shore Private Hospital. HREC reference NSPHEC 2013-002.
Results
Baseline Characteristics
Of the 20 patients who were enrolled in the study all 20 completed follow-up including evaluation and MRI. Eight patients were female. The patients’ average age at the time of surgery was 50.9 ± 7.7 year (range 37-67 years). Pre-operative forward elevation was 129±39 degrees (range 60-180 degrees). All patients underwent a subacromial decompression at the time of surgery. Seventeen patients had a biceps tenodesis performed concurrently and two patients had a distal clavicle excision performed concurrently. The length of follow up averaged 6.2 ± 0.5 months (range 6-8 months).
Functional Outcomes
As expected following rotator cuff repair, patient-rated outcome measures improved (table I). ASES scores increased an average of 32.2 points (p<.001) and ranged from an 8 to 73 point increase. Normalized constant scores increased on average 31.5 points (p<.001) and ranged from 3 to 68 point increase. VR 36 physical scores improved on average 11.8 points (p<.001) and ranged from 1.3 to 25.7 point increase. There was no difference in VR 36 mental scores (p =.60).
Physical exam findings improved following rotator cuff repair. Forward elevation improved from 129±39 degrees to 167±23 degrees (p<.001). Abduction did not demonstrate significant change (p=0.24). Post-operative abduction strength measured by dynamometer was 5.4±2.7 kg.
Repair Integrity
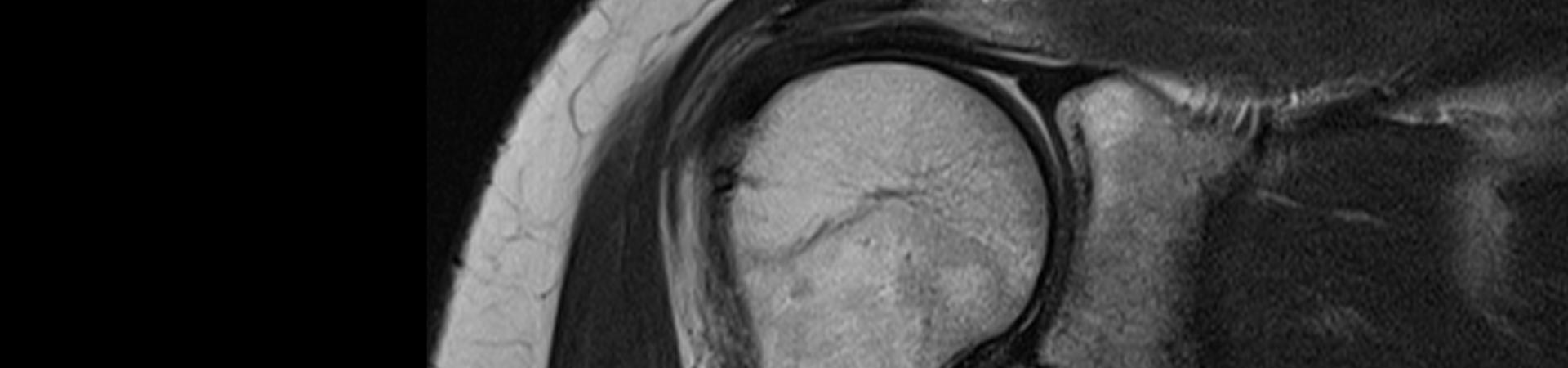
Post-operative MRI results demonstrated clinical healing (Sugaya score of 1-3) in 19 patients and a failed repair in one patient with a Sugaya score of 5 (see table II). This represents a healing rate of 95%. No patients had development or progression fatty degeneration of any of the rotator cuff muscles on follow-up MRI. Figure 1 demonstrates an intact rotator cuff repair as seen on post-operative MRI.
With these results, we have concluded that early sling discontinuation following double row rotator cuff repair may be an acceptable option for small non-retracted rotator cuff tears in properly selected patients with a high likelihood of healing.