Rationale
The rationale for this study was to evaluate our operative outcomes for distal biceps repairs utilising a one incision technique, and compare these outcomes to pre-morbid function and current literature.
Objectives
To retrospectively assess a cohort of patients at 1 year or more after surgery for distal biceps repair, reviewing functional outcomes including strength and range of motion measures and compare these with current literature.
Design
This study combined retrospective medical records review with long term clinical follow up.
Study Procedure
Relevant patients were identified from surgical log books. A retrospective medical record review was undertaken. Information utilised included routine functional outcome measures recorded at time of follow up. Patients were not asked to undergo any investigations specifically for this research project – the study design was equivalent to a routine clinical visit that many of these patients already attend regularly. Data analysis documented the findings of the long-term follow up. Correlations with pre-operative presentations and surgical treatment were examined.
Results
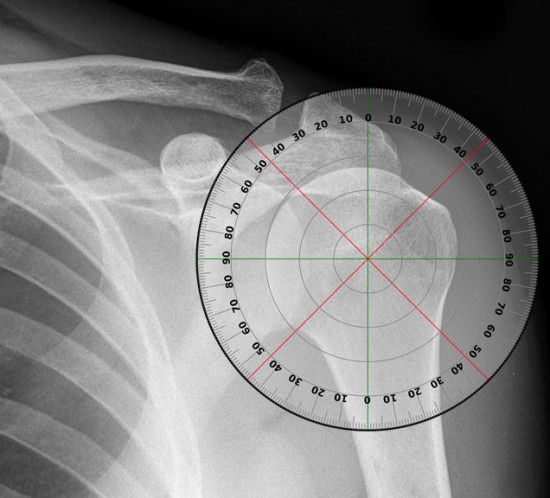
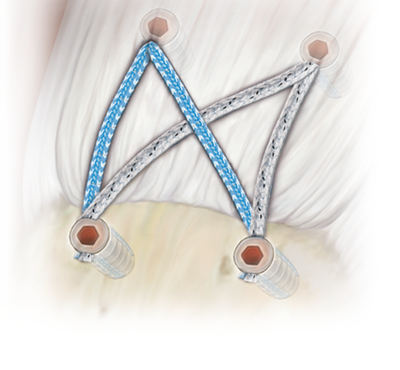
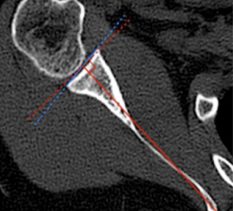
Ten unpaired cadavers (6 left, 4 right) were used. With the guide wire inserted through the centre of the tuberosity the mean distance from exit point to the PIN was 7.33mm (95 CI% 5.61 to 9.05). With the guide wire inserted at a more proximal entry point, the mean distance from the exit point to the PIN was 10.92mm (95 CI% 9.37 to 12.47). This results represents a statistically significant (P = 0.0036) difference between the two methods.
Strength and ROM measurements for a total of ten patients (all male) were available for analysis. Mean age was 49.2 years (range 34 to 61). In four participants, the repair was performed on the dominant arm. Supination and flexion strengths were on average 83% and 90% of the uninjured side respectively. There was a mean of 1.5° loss of flexion and 0° loss of extension. Pronation loss was 0.5° on average. Supination loss was 4.5° on average. All 10 patients had at least 1 year follow up with no complications reported including nerve palsies, fractures, wound infections or revisions The mean DASH score was calculated to be 6.3 on a scale of 0-100 (with higher numbers indicating increased functional impairment).
In this study, we have demonstrated a safer entry point, in regards to the PIN, for insertion of the radial guide wire during distal biceps tendon repair. The more proximal entry point represents a reliable and safe alternative for this type of repair.